Since March 2020, economists throughout the world have conducted studies related to COVID-19. Proposed policy options include restrictions on activity (voluntary restraint and business shutdowns in Japan), testing and quarantine, selective restrictions on activity for elderly people, and on-and-off restrictions on activity.
Papers by Professor Martin Eichenbaum of Northwestern University in the United States and other economists theoretically indicate that fears of infection restrict human activity, leading to economic decline. Weekly consumption is estimated to drop as much as 17% if humans voluntarily reduce consumption and work to avoid infection.
Professor Oliver Holtemoeller of the Halle Institute for Economic Research in Germany argues that large-scale testing and the quarantined recovery of COVID-19-positive people over the long term after short-term restrictions on activity would be an optimum option. If testing costs (including the problem of false positives or negatives) increase, however, large-scale testing and quarantine may not necessarily be an optimum option.
A paper by Professor Daron Acemoglu of the Massachusetts Institute of Technology and others argues that an optimum policy would continue elderly people's voluntary restraint over the long term while quickly lifting restrictions on young people. Professor Tai Takahashi of the International University of Health and Welfare has made a similar argument.
♦ ♦ ♦
Polymerase chain reaction (PCR) and other testing capacity, including the maximum daily number of tests, are remarkably limited in Japan. The maximum daily number of tests in Japan is 20,000 against 400,000 in the United States and 150,000 in Germany. The remarkably limited testing capacity has led people to fear community-acquired infections and restrict consumption and other economic activity.
However, Japanese infectious disease experts argue that cluster infection measures are more effective than random testing, given COVID-19 transmission behavior. According to the Analysis of the Response to the Novel Coronavirus Disease and Recommendations formulated by the Expert Meeting on the Novel Coronavirus Disease Control on May 29, COVID-19 infections spread as some infected people cause cluster infections when some conditions, including the three C's (closed spaces, crowded spaces, and close-contact settings), are met. The spread of COVID-19 differs from the spread of influenza in which all infected people equally cause infection (see a figure below), as indicated by the report.
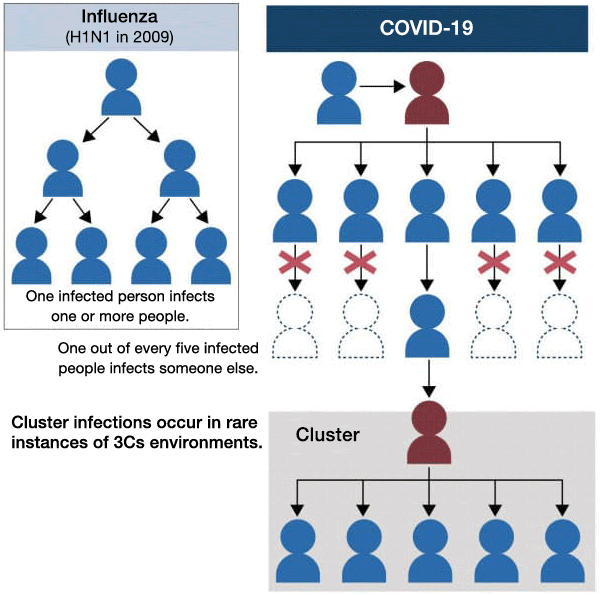
In the case of a virus with such transmission behavior, it is said to be efficient to find clusters, trace those having had close contacts with infected people, and identify three C's sites. It is pointed out that as 80% of COVID-19 infected people recover from the virus without infecting anyone else, random testing to find infected people is not so useful in preventing infections from spreading. It is hoped that this new finding will be highly regarded by infectious disease experts around the world.
Proactive epidemiological research guidelines of Japan's National Institute of Infectious diseases (May 29) define a close contact person as a person who had close contact with an infected person up to two days before the infected person become symptomatic, excluding anyone who had close contact with the infected person at an earlier time. Regarding an asymptomatic infected person, a close contact person should have had close contact with the infected person up to two days before testing under the guidelines. The World Health Organization has concluded that the virus is the most infectious just before and after an infected person becomes symptomatic. Although the narrower Japanese definition is inevitable under the limited testing capacity, the definition should be widened, given that the virus is infectious even more than two days before the development of symptoms.
Japan boasts retrospective tracing of people that had contact with COVID-19 infected persons, in which tracing covers up to 14 days before the development of symptoms. However, local authorities are inconsistent in their decisions on whether to conduct PCR or other tests for asymptomatic people. In principle, suspected infection sources among those who had contact with infected people up to 14 days before the development of symptoms should be tested as widely as possible, even in the absence of symptoms, to prevent cluster infections. This point should be communicated thoroughly nationwide. To this end, the government should increase funding, human, and other resources to enhance testing and treatment capacity to allow medical doctors to immediately conduct testing based on their own decisions.
Given that community-acquired infections have spread to some extent in Japan and that Japan has no choice but to accept more foreign visitors in the future, arrangements should be developed for even lightly symptomatic people to immediately undergo PCR or antigen tests based on decisions by medical doctors to quickly find signs of any cluster infections.
In a winter influenza epidemic period (when infections peak at 100,000 to 300,000 persons daily), all suspected COVID-19 patients should undergo PCR tests, because influenza and COVID-19 symptoms are difficult to distinguish. If not, there may be chaos on the front lines of the healthcare system. Such chaos may lead the government to again declare a state of emergency. To avoid such a development, Japan should secure a daily testing capacity of 200,000 persons by winter.
♦ ♦ ♦
Stipulating the numerical target for increasing testing capacity to 200,000 tests per day by the end of November is significant for two reasons. First, such a numerical target for medical treatments and tests can reduce sources of uncertainty and increase security, helping to vitalize the economy by making it easier for consumers and enterprises to set action plans. Second, no one can develop human resources development or goods procurement plans without numerical targets.
Providing objective explanations of the need to take necessary measures (such as another declaration of a state of emergency) gains the understanding of the population by increasing transparency in a policymaking process and is indispensable for the legitimacy of any policy. -The abovementioned Analysis of the Response to the Novel Coronavirus Disease and Recommendations raises some related issues.
A factor that prompted the declaration of the state of emergency to be issued in Japan was the potential collapse of healthcare systems. However, some news reports state that data regarding the number of people hospitalized for COVID-19 in Tokyo were incorrect. To enhance healthcare systems, the government must verify how strained healthcare systems were at that time and identify healthcare bottlenecks.
First, the government must accurately identify the risks of severe symptoms and deaths for COVID-19-infected people. When requesting that people impose costly restrictions on activity, the government is required to explain relevant risks and secure the transparency of its policymaking process to obtain people's understanding. The government may have to indicate not only the total number of deaths but also high-risk groups, based on an analysis of ages and underlying diseases. Such information is important for designing restrictions on activity.
Additionally, the process by which symptoms increase in severity must be analyzed in more detail. What are effective medical treatments for each of the phases of the development of symptoms, moderate symptoms, severe symptoms, and recuperation? Some healthcare providers have testified that reduction of fever and nutritional care to prevent loss of physical strength can help prevent severe symptoms in COVID-19. The government should immediately organize and publish current, accurate information to facilitate the national understanding of COVID-19 countermeasures.
To prepare for a second wave of COVID-19 infections and an influenza outbreak, and to ease immigration regulations and normalize economic and social activity, the government should publish and implement plans including quantitative targets for several months or one year from now. In addition, it should increase people's security and confidence by clarifying a transparent policymaking process in which it requests the voluntary restraint of the populace and shutdowns of businesses if healthcare systems are strained to the extreme.* Translated by RIETI.
June 17, 2020 Nihon Keizai Shimbun


