Requiring COVID-19 vaccination as a condition of employment is a controversial policy. This column asks whether the resulting benefits, in terms of illness and deaths averted, exceed the direct costs, focusing on the impacts of four national US mandates. The authors find that the net benefits depend on the subsequent evolution of the pandemic. If the pandemic grows rapidly, the benefits of mandates likely far exceed their costs; if the pandemic is waning, the opposite is likely the case. Under any scenario, comparison with the effects of other policies is needed to determine the best approach.
In 2021, the Biden administration issued several mandates requiring COVID-19 vaccinations, including mandates covering US federal employees, US federal contractors, federally funded health care providers, and certain private sector workers (Biden 2021a, 2021b, OSHA 2021, CMS 2021). These mandates have been challenged in court; some have been halted or delayed. Substantial attention has been paid to the net benefits of lockdowns and other policies (e.g. Greenstone and Nigam 2020, Thunström et al. 2020). However, rigorous assessment of the costs and benefits has accompanied neither the decisions to impose these vaccination mandates nor the decisions to overturn them. Such assessment is needed to inform future decisions to implement mandates at state, local, and national levels globally and to support comparison of mandates with other protective measures.
To help fill this gap, we estimate the direct costs and health-related benefits that would have accrued if US vaccination mandates had been implemented as intended (Ferranna et al. 2022). Compared with the January 2022 vaccination rates, we find that the mandates could have led to 15.8 million additional vaccinated individuals, increasing the overall proportion of the fully vaccinated US population from 64% to 68%. If the pandemic had then grown, the benefits would have reached almost $20,000 per additional vaccinated individual, with more than 20,000 total deaths averted over a six-month period. If the pandemic had instead faded, existing vaccination-acquired or infection-acquired immunity would have provided sufficient protection and the mandates’ benefits would have been unlikely to exceed their costs. Thus, mandates may be most useful when the consequences of inaction are catastrophic.
Our approach follows the conventional benefit-cost analysis framework (HHS 2016). It includes four components. First, we estimate the change in the number of vaccinated people that is attributable to the mandates, comparing the ‘without mandate’ baseline with ‘with mandate’ conditions. We rely on data from several sources on vaccine uptake and vaccine hesitancy to develop these estimates. Second, we estimate the direct costs of the mandates, focusing on those associated with vaccine administration and time losses associated with adverse reactions. For each additional person who is fully vaccinated, we find that these costs likely total about $340.
Third, we estimate the change in the number of COVID-19 nonfatal cases and deaths that is attributable to the change in vaccination rates, considering the effects on those whose vaccination status changes and on other members of the population. In this step, we use a standard compartmental epidemiological model. Calibration of the model requires estimating several parameters. The most important ones relate to the characteristics of the vaccine itself (its effectiveness and duration), the initial condition of the population (e.g. the proportion susceptible, infectious, or recovered), and the reproduction number (the infectiousness of the virus, given infection- and vaccination-acquired immunity and other measures to control its spread). Fourth, we estimate the monetary value of the illnesses and deaths averted, accounting for both individuals’ willingness to pay to avoid these risks and averted medical costs (Robinson et al. 2021, 2022).
Our viewpoint is ex ante; we predict what might have occurred had the mandates been implemented as planned, accounting for uncertainty regarding the future course of the pandemic. We consider impacts over a six-month period, given evidence that vaccine protection begins to wane after this time.
Net benefits depend heavily on the pandemic pathway. We consider two illustrative scenarios. Under the first, a large share of the population has infection- or vaccination-acquired immunity; only a small surge of infections occurs before new cases rapidly diminish, and as a result the health benefits of the mandates are limited. Under the second, we assume that a new, more infectious variant emerges for which existing vaccines and past infection are less protective. Figure 1 illustrates the number of active infections under each scenario without the mandates.
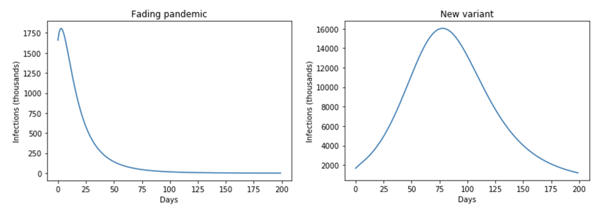
[Click to enlarge]
Increasing the number of fully vaccinated individuals by 15.8 million has very different effects under these two scenarios. In each case, the costs are the same ($5.4 billion). However, with a new, more transmissible variant, against which previous infections and vaccination are less effective, the total value of benefits increases by almost a factor of 40. As Table 1 illustrates, the difference in benefits alters the likelihood that net benefits will be positive.
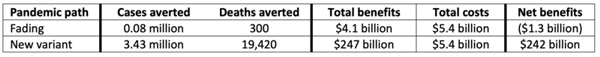
[Click to enlarge]
Our estimates likely understate the net benefits of the mandates given that we limit the analysis to a six-month time frame and consider a limited set of effects (Bloom et al. 2021). Additional benefits of increased vaccination may include reducing public and private expenditures on outbreak containment and response, lowering the likelihood that other variants will emerge, increasing the resources available to treat other health conditions, and improving mental health. Increased vaccination rates may also improve educational outcomes by permitting schools to stay open (Asakawa and Ohtake 2022), spur economic activity and growth by reducing business closures and increasing consumer confidence and demand (Hansen and Mano 2022), and improve social wellbeing by decreasing isolation. Vaccine mandates may also provide more equitable protection by addressing barriers to increased vaccination rates among low-income and otherwise disadvantaged populations.
However, these mandates raise concerns about requiring individuals to undertake measures that they would not willingly undertake on their own. Other approaches to increasing vaccination rates (e.g. Bennett et al. 2022) and protecting against transmission (e.g. masking, social distancing, and ventilation and filtration) may receive more public support. Comparison with other policies is needed to determine which are likely to be most protective, effective, equitable, and cost-beneficial.
This article first appeared on VoxEU on December 20, 2022. Reproduced with permission.






