Although Japan has once again rescheduled the plan to raise the consumption tax rate, this time from April 2017 to October 2019, Prime Minister Shinzo Abe remains committed to the fiscal reform goal of bringing the primary balance of the central and local governments into a surplus by FY2020. With the door to any tax hike closed for the time being, the focus of debate on Japan's fiscal reform is on growth measures and expenditure reform particularly in the area of social security system.
One of the areas requiring review is the design of public health insurance coverage for medical treatment and medications. We need to approach this from the perspective of seeking to achieve two seemingly conflicting goals—i.e., the creation of new industries and the consolidation of public finance—while maintaining the framework of the existing universal health insurance system, an internationally acclaimed scheme.
Using IMS Japan's big data covering almost all trade in medicinal products in Japan, we have attempted to estimate and analyze the effects of possible options for changing insurance coverage for medications. In this article, I would like to outline our pro-forma calculation results for two possible reform plans.
♦ ♦ ♦
In redesigning public health insurance coverage as a way to curb soaring government medical expenditures to a sustainable level, we can take the following two reform plans: 1) raising the copayment rates and 2) changing the government-set prices of medical services and medications as well as the scope of insurance coverage.
Our first reform plan, which models after the French health insurance system, calls for introducing a new medication copayment system that sets different copayment rates depending on the severity of the diseases to which medications are applied and the efficacy of medications in treatment to replace the current age-based system (Reform Plan 1). Under the current system, the standard copayment rate is set at 30%, but reduced rates apply to certain age groups, i.e., 20% for preschool children and elderly people aged 70-74, and 10% for those aged 75 and above. The second one calls for changing the government-set medication prices to better reflect the severity of the diseases to which medications are applied and the efficacy of medications in treatment but maintains the current age-based copayment system (Reform Plan 2).
One of the most important roles played by a public health insurance system is to protect insured people and their households from the risk of bankruptcy or impoverishment resulting from the treatment of serious illness. In planning and implementing steps to reform the system, it is necessary to give due consideration to the resulting potential burdens on the insured and determine the magnitude of their impact.
Meanwhile, under Japan's current public health insurance system, the copayment rate applicable to medications that are indispensable to or known to be highly effective in the treatment of serious diseases is no different from that for medications that are not indispensable or those for which generic alternatives are available. This leaves the question of how much of the cost of those medications, which differ significantly in the degree to which they are useful and indispensable, should be borne by public insurance respectively.
In order to promote innovation such as the development of innovative drugs and medical technologies, successful innovators should be able to reap reasonable rewards. However, this does not go well with Japan's other important endeavor to consolidate public finance. Our aim in this article is to show that it is possible to provide greater insurance coverage for innovative and effective medications and alleviate the financial burden of patients with serious illness by applying different copayment rates to medications based on their usefulness and indispensability.
Cases of other countries serve as a good reference in reforming the copayment system for medications. In France, for instance, copayment rates for medications vary according to the level of therapeutic contribution and usefulness. Specifically, patients pay none of the cost for expensive drugs for which no alternatives are available, 35% for ordinary prescription drugs, 70% for over-the-counter drugs such as gastrointestinal drugs, 85% for drugs deemed not useful, and 100% for vitamins and tonics. Meanwhile, in Sweden, a country known for its generous healthcare welfare systems, all patients except for children bear the full cost of medications up to 900 krona (approximately 10,000 yen) per year regardless of the type of drugs, plus a designated percentage of any amount in excess of the threshold.
♦ ♦ ♦
Drawing on the case of France and with the help of a group of specialists, we classified insurance-covered prescription drugs in Japan into three categories: (A) drugs for serious illness that may result in death or serious aftereffects, (B) drugs for which no generic alternatives are available although not meant for serious illness, and (C) other drugs. Here we set the copayment rate for drugs classified into (A) at 0% to ensure generous protection for those with serious illness, and that for (C) at 70% in a bid to promote the use of cheaper generic alternatives wherever available, while keeping the rate for (B) unchanged from the current 30%. Based on those assumptions, we performed pro forma calculations to estimate the resulting changes in benefit amounts (see Figure).
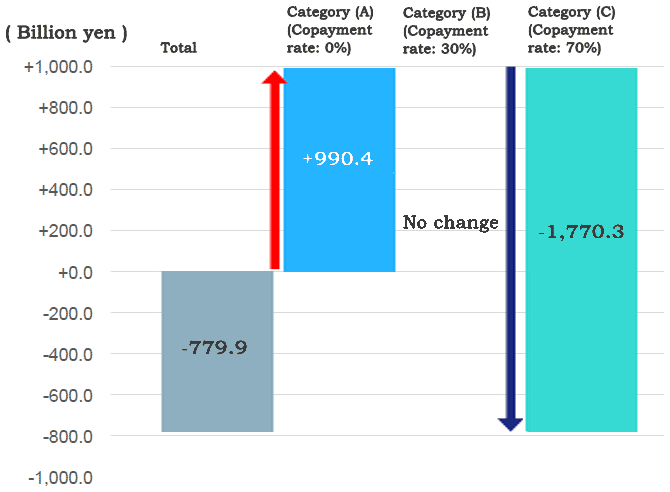
The results of our calculations suggest that it is possible to provide greater insurance coverage for medications that are more indispensable and useful without compromising the level of sustainability planned under the current system. The proposed changes to copayment rates would reduce the amount of insurance benefits payable to cover medications by about 780 billion yen.
It should be noted that these calculations are rough estimates and do not completely reflect the effects of the High-Cost Medical Care Benefit System, a reimbursement program to cover any amount in excess of the designated maximum monthly copay amount, and changes in demand for medical services resulting from the proposed changes to the copayment rates. Those factors require separate consideration.
The reform plan to change the existing age-based copayment system would face intense opposition from elderly people whose copayment rates are relatively low under the current system. Thus, we estimated the effects of Reform Plan 2 that would maintain the current copayment rates and instead change the prices of medications based on the degree of necessity and usefulness.
Under the current system for the listing of drugs on the government-set drug price list and hence subject to public insurance coverage is done on a brand-by-brand basis in most cases. A typical explanation is that such a brand-by-brand approach has its advantage in its effect to properly reflect market prices in government-set prices, thereby eliminating the room for medical institutions and dispensing pharmacies to make bountiful profits on the difference between government-set prices at which they are paid and the corresponding cost prices. In reality, however, various opaque business practices—such as rebate payments from pharmaceutical companies to wholesalers and provisional delivery without price agreement between wholesalers and medical institutions—are still in place, and it is quite difficult to capture the true picture of market prices.
Furthermore, revisions to the government-set drug prices take place only once every two years. Thus, even when the market price of a certain drug goes down, the government-set price remains unchanged for some time, possibly resulting in an inefficient allocation of resources that represents a significant diversion from the actual trend of market prices. It is necessary to eliminate those factors to enable the allocation of more resources to more effective and useful drugs and thereby encourage the development of innovative drugs.
In Reform Plan 2, we keep the copayment rates unchanged from those under the current system but change the government-set prices. Using the same categories as those for Reform Plan 1, we set prices for drugs in Categories (A), (B), and (C) at 1.05 times, 1.03 times, and 0.97 times the current levels respectively, and estimated the financial impact of the price changes. This has the same effect as introducing multiple, differentiated reduction rates in drug price adjustments, instead of applying a uniform reduction rate of 2% as under the current rules. The results of our calculations for Reform Plan 2 also show that it is possible to reduce the amount of insurance benefits payable to cover medications by approximately 800 billion yen while allocating more resources to more effective and useful drugs.
♦ ♦ ♦
The scope of our analysis is limited to the insurance coverage of medications. However, as more health information technologies—including the national database containing data on health checks and health insurance claims—are adopted, and when the necessary hard and soft infrastructure for use of healthcare big data are made available, it will become possible to conduct a more precise analysis of the government-set prices of medical services. When this happens, it will enable more effective and efficient pricing of medical services based on scientific evidence.
Financial resources saved by implementing reform such as those proposed above can be utilized, in part, to help restore the nation's fiscal health. However, it is also important to allocate them to promote the creation of new industries. The global pharmaceutical market—worth approximately 100 trillion yen in 2015—is expected to grow at a pace of 3% to 6% per annum in the next five years. Japanese pharmaceutical startups could make a significant contribution to two of the government's policy goals—i.e., the development of new industries and the creation of jobs—if they have greater chances to advance into the global market by using the domestic market as a stepping stone.
From the perspective of pursuing two policy goals—i.e., the creation of new industries and fiscal consolidation—at the same time, it is hoped that the government will further facilitate comprehensive use of big data in the area of medical services and make steady progress in healthcare reform.
* Translated by RIETI.
November 10, 2016 Nihon Keizai Shimbun



